

ACT-DRG-Optimizer is designed for use by Healthcare providers where the healthcare professionals are documenting the patients diagnosis using a coding system based on a locally disease classification adapted from the WHO ‘International Statistical Classification of Diseases and Related Health Problems’, Tenth Revision (ICD-10). The Healthcare provider is fully or partly funded using a case-mix classification system that groups together patients who are similar clinically in terms of diagnosis (and treatment).
To illustrate the principle function of ACT-DRG-Optimizer consider the following very simplified cases. In these cases the case-mix classification system is a locally modified Diagnose Related Grouping system used in Scandinavia (NORD-DRG).
In all cases a ‘standard patient’ is used. It is a male born on the 1st of January 1950 and he is admitted on January the 29th 2006 and he is discharged after 6 days.
The patient is treated for hyperkalemia.
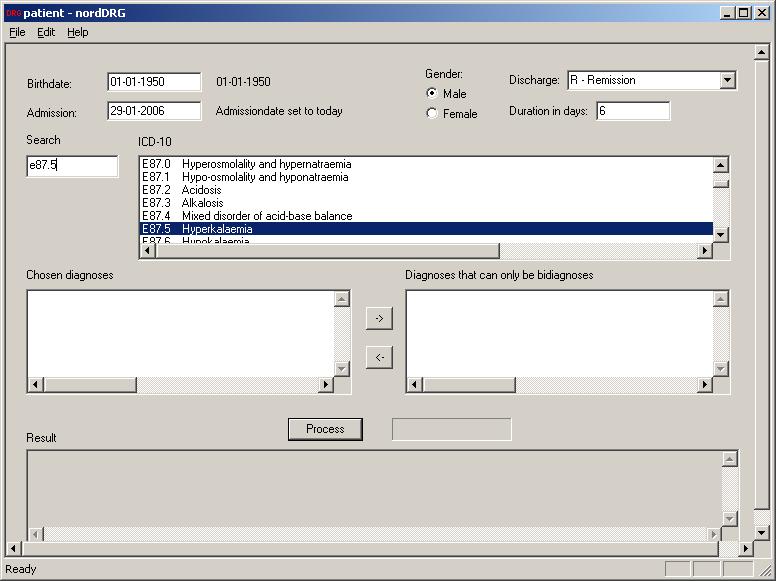
The birth date, the sex, admission date (default is current date), mode of discharge and duration of stay is entered. Then the ICD-10 diagnosis code E87.5 is entered. The corresponding diagnosis hyperkalemia is now displayed in the ICD-10 box. The diagnosis is confirmed by double clicking it with the left mouse button.
When the diagnosis appears in the ‘Chosen diagnoses’- box the button <Process> is activated. The result of the DRG-grouping is displayed in the ‘Result’-box.
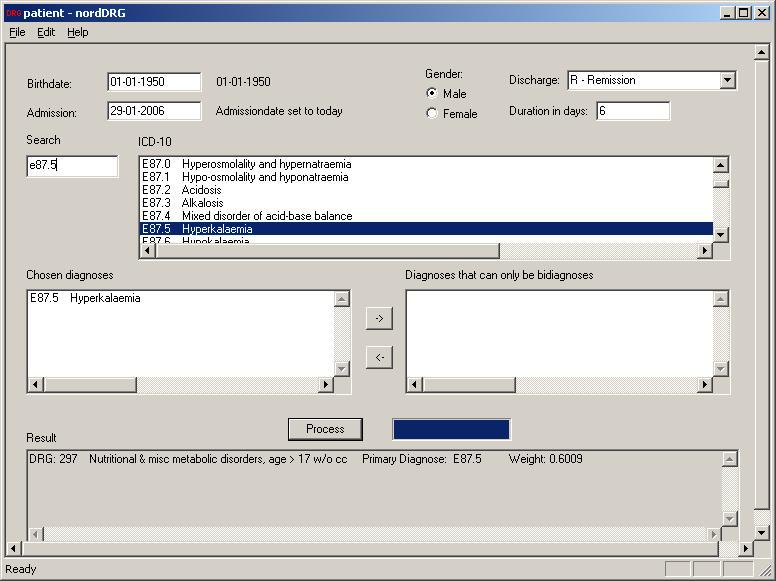
The diagnosis Hyperkalemia belongs to DRG group 297 labeled ‘Nutritional and misc metabolic disorders in patient older than 17 years without complications’. It has a weight (DRG-points) of 0.6009.
Let’s say that the Healthcare Provider is paid 4000 € per DRG-point. For the Healthcare provider this patient represents a value of approximately 2400 € (4000 * 0.6).
The patient is now a bit more complicated and is also suffering from increased coughing due to bronchitis (Chronic obstructive pulmonary disease). The patient is obviously treated for both conditions. Which of the diagnosis should the Healthcare provider be funded for?
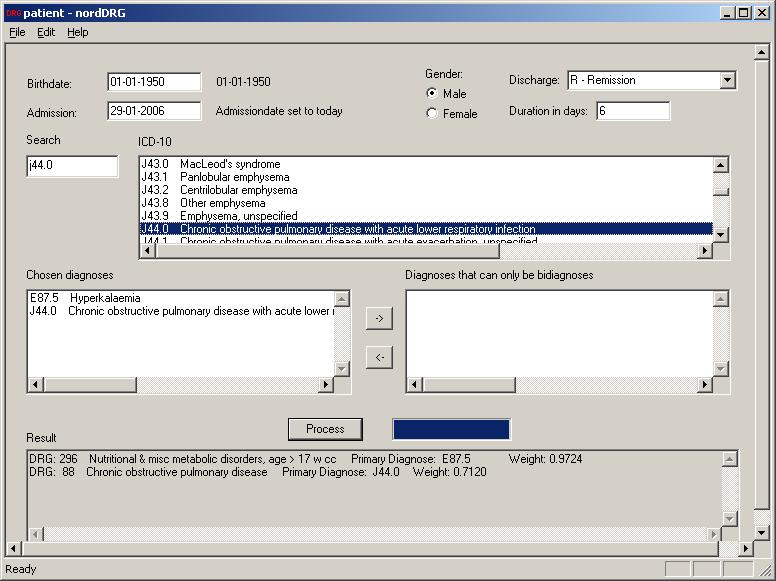
The diagnosis J44.0 ‘Chronic obstructive pulmonary disease with acute lower respiratory infection’ is entered and processed as an additional main diagnosis. It can now be read in the ‘Result’-box that the previous diagnoses hyperkalemia now is grouped in a new DRG-group namely 296 ‘with complication’ (w cc). The reason is that the COPD diagnosis (grouped as DRG-group 88) complicates hyperkalemia changing it from DRG group 297 to 296.
Note that the diagnosis in the ‘Result’-box is ranked by their DRG-Weight.
The weight has now increased to 0.9724 and the value has now increased to approximately 3900 € simply because the patient has a complicating diagnosis. This case illustrates the importance of recording all diagnoses.
The case is now even more complicated. Besides hyperkalemia and COPD the patient has insulin treated diabetes and several of diabetes’ companions, such as hypertension with decreased kidney function and high blood fats. He even sufferes from a myocradial infarction (MI).
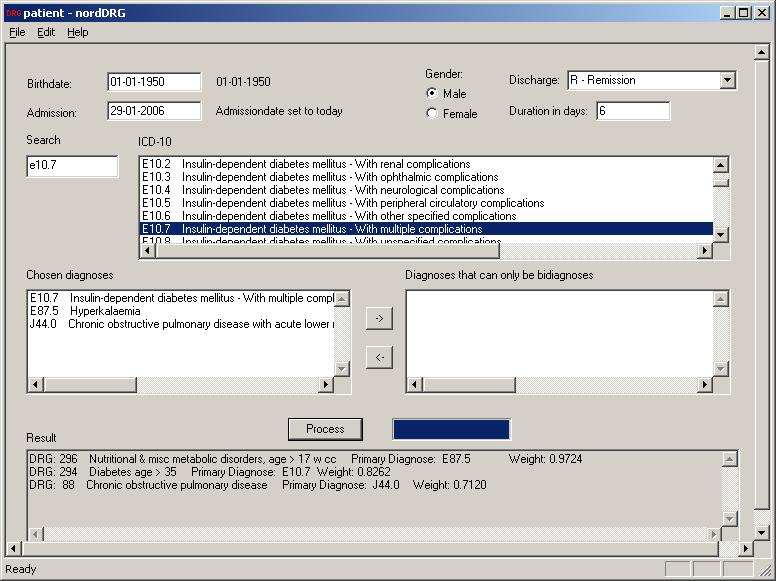
One way of looking at this case is simply by viewing the MI as primarily a consequence of his two chronic conditions namely diabetes and COPD. Consequently the diagnose MI is omitted. The ‘Result’-box shows that it still will be most economical efficient to set the main diagnosis as hyperkalemia.
Another way of looking at the patient is of cause to view the acute myocardial infarction as one of the main reasons for the hospitalization. Besides receiving treatment for the MI, the patient also receives treatment for his kidney failure and his diabetes. Hence all three of them are categorized as main-diagnoses.
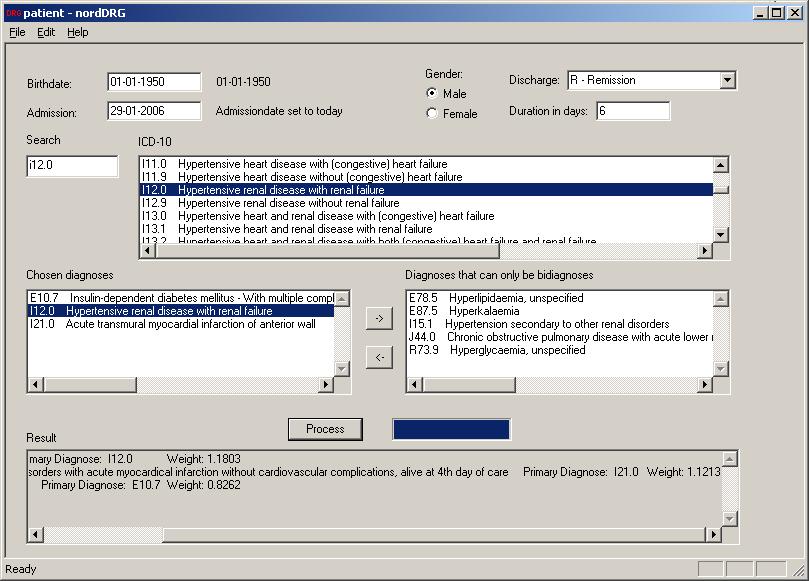
Using this argument the hyperkalemia is a consequence of the kidney failure and should be categorized as a bi-diagnosis. Likewise the rest of the diagnoses are categorized as bi-diagnoses. Diabetes is from a pathological point of view probably the main cause behind it all.
It can be debated medically, which of the three main-diagnoses is the hen and which is the egg. From a pecuniary point of view – as revealed in the ‘Result’ box – one should use the kidney failure as the principle diagnosis since it represents approximately 5.25% higher value than the MI-diagnosis and approximately 43% higher value than the diabetes-diagnosis.
ACT-DRG-Optimizer is designed to aid in the process of setting optimal diagnosis in various patient administrative systems without interfering with the processes involved in the use of medical diagnosis.
Setting the right medical diagnosis is entirely a task for the medical profession. Translating this medical diagnosis into the best suited ICD-10 diagnosis is also mostly a task for the medical profession, however choosing the most optimal diagnosis from a purely administrative point of view as is the case with DRG is hardly a task that belongs to the medical profession.
By using the ACT-DRG-Optimizer this translation and optimization is partly automated. The medical professions’ only task is to list all the possible main- and bi-diagnosis believed to be medically correct. Then the ACT-DRG-Optimizer finds the most optimal DRG-group to report into the financial systems of the health care provider.
ACT-DRG-Optimizer can be fitted to the individual health care providers needs.
It can be delivered as a stand-alone solution or for multi-users in a network. It can be integrated in the health care provider’s EPR-system and/or into the administrative system.
ACT-DRG-Optimizer can operate with all standard database software.
We also deliver tools for analyzing the diagnosis-settings within an organization aiming at early detection of changes in the diagnosis-setting culture of an organization – to avoid critical DRG-creep. The tool can either be based on analyzing the historical data within the organization or as benchmarking against another organization.
Based on more advanced statistical analysis our solutions can of cause also be very helpful for the payer when analyzing the claims from the providers.
For further information visit our website www.act-consult.com or mailto:info@act-consult.com